Dr Manish Singhal - The best Cancer Specialist in Delhi
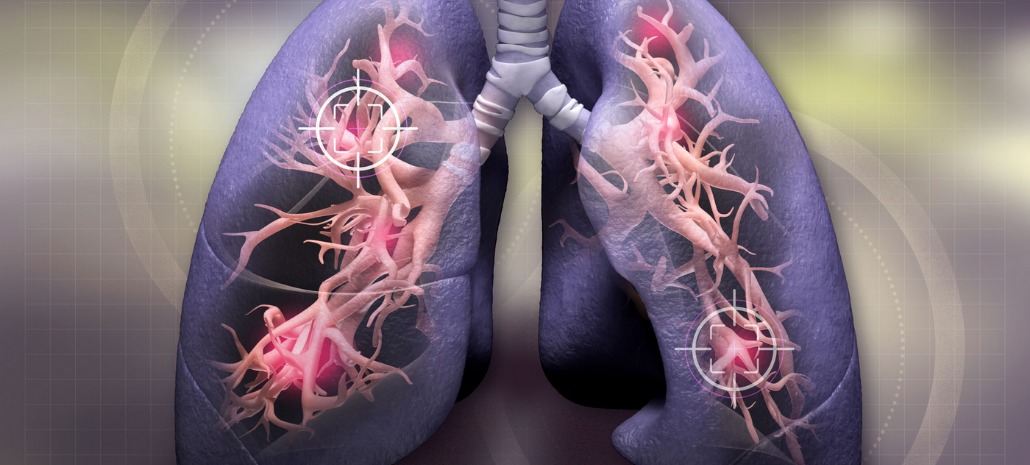
Advanced Non Small Cell Lung Cancer Targeted Therapy: Current State VS Future Trends
Lung cancer is one of the most common cancers, accounting for 84% of all cancers. 2 million new cases and 1.7+ million deaths were attributed to lung cancer in 2018 alone.
Non-small cell lung cancer and small cell lung cancer are the two major types of lung cancers. Out of the two, non-small cell lung cancer is the most common accounting for 9 out of 10 lung cancer cases.
In recent years, the world has seen a paradigm shift in the status, treatment, and management of non-small-cell lung cancer.
While experiential chemotherapy with a platinum-doublet remains the gold standard for advanced NSCLC without a known driver mutation, targeted therapy is the new kid in the block, pushing boundaries of improving patient outcomes & quality of life.
For some NSCLC patients with actionable mutations, targeted therapy is providing durable responses. Multiple advances in molecular and immunohistochemical techniques in recent years have made it possible to lead lung cancer into a new era of personalized medicine. This has led to patients getting individualized treatment based on such markers.
In this blog, we will dive into the current trends of targeted therapy in advanced non-small-cell lung cancer.
Targeted therapy in non-small-cell lung cancer-Today & tomorrow
EGFR inhibitors
Currently, Osimertinib is the standard of care for untreated EGFR mutant (ex19del or L858R) advanced NSCLC because of its superior efficacy and enhanced tolerability.
However, there is no targeted therapy for cases that have progressed after osimertinib administration.
Presently certain studies are going on to address the same. Lazertinib is being studied and has shown 57.9% overall response with 89.5% disease control in certain patients with progression. In the case of Olmutinib, 46.3% of patients in a study had confirmed an objective response with an 86.4% disease control rate. Nazartinib is being studied individually and in combination with gefitinib and trametinib. Aflutinib, on the other hand, has gone through previous trials and is going through a phase II trial that is still enrolling.
4th generation of EGFR TKIs are currently being studied to overcome C797S-the most significant on-target resistance mechanism to osimertinib.
BDTX-189 is being studied in patients with advanced solid cancers including EGFR mutant NSCLC.
CLN-081 (TAS6417) is a potent pan-mutation-selective EGFR inhibitor with a broad therapeutic window. Preclinical studies have been done and now it is in phase I/II trial.
Other 4th generation EGFR TKIs include DZD9008, Tarloxotinib, Amivantamab, Poziotinib, and Mobocertinib. All in different phases of multiple clinical trials.
EGFR therapy is also often studied in combination with other targeted agents. Amivantamab is being evaluated as a monotherapy or combination with Lazertinib or chemotherapy for certain types of NSCLC. Osimertinib and savolitinib are also being studied in combination.
ALK inhibitors
3–7% of NSCLC patients have rearrangements in the anaplastic lymphoma kinase (ALK). While Crizotinib was the first FDA-approved ALK inhibitor, since then, many others like ceritinib, alectinib, brigatinib, and lorlatinib have been approved.
First-line brigatinib was proven superior in a trial. First-line lorlatinib was evaluated and more grade 3 or 4 adverse events were found in it. SAF-189 s, a novel selective ALK inhibitor with CNS penetration was also evaluated in a clinical study. TQ-B3101 was found to inhibit ALK, ROS1, and MET. TPX-0131, a next-gen ALK inhibitor, is being currently evaluated.
Brigatinib is being evaluated in combination with bevacizumab, and alectinib is under investigation in combination with cobimetinib.
Finally, the National Cancer Institute’s ALK Master Protocol is set to prospectively match patients to appropriate ALK TKIs based on the underlying ALK-resistance mutation.
MET inhibitors
Currently, two FDA-approved MET inhibitors can be used as first-line therapy in metastatic NSCLC with MET exon 14 skipping mutations.
FDA has approved capmatinib as the first-line in patients with MET exon 14 skipping mutations based on the GEOMETRY mono-1 trial.
Capmatinib was approved as the first-line treatment in patients with MET exon 14 skipping mutations. Tepotinib is a highly selective MET inhibitor that is currently being evaluated in a phase II trial.
In another interesting trial, it was seen that a mixture of 2 humanized antibodies-Sym015, triggers MET degradation. Further trials are ongoing.
Glumetinib, a selective MET inhibitor, is another well-tolerated targeted therapy in certain advanced NSCLCs. A phase I trial is still underway. Multiple others like APL-101 (a highly selective small-molecule c-Met inhibitor) and REGN5093 (a human bispecific antibody) are also being studied.
RET inhibitors
Non-small-cell lung cancer with RET fusion comes with a high risk of brain metastasis. Previously, cabozantinib and vandetanib were used with modest benefits but significant toxicity. However, now the USFDA has approved selpercatinib and pralsetinib after great phase II results.
Selpercatinib, a highly selective small-molecule inhibitor of RET kinase, was approved for NSCLC with RET fusion after a phase II trial with 105 patients. The phase III trial comparing it to standard frontline treatment is underway.
The USFDA approved pralsetinib for RET-fusion positive NSCLC based with or without any prior therapy based on the phase I/II ARROW trial. A phase III trial is currently enrolling patients.
TPX-0046 is another next-gen RET inhibitor being studied. BOS172738 is a highly potent and selective RET inhibitor under investigation.
BRAF/MEK inhibitors
BRAF mutations are uncommon in NSCLC and seen in less than 5% of NSCLC patients. Today a combination of dabrafenib and trametinib is preferred by most cancer specialists where dabrafenib inhibits BRAF V600E mutations, and trametinib inhibits MEK.
Oral LXH254 was effective in the phase I trial and is currently in phase IB. ABM-1310, an investigational, oral, small-molecule BRAF inhibitor, is also in a first-in-human phase I trial.
ROS1 inhibitors
The ROS1 rearrangements were first observed in 2007. Its exact function is unknown, but its highest expression was seen in normal lung tissue.
Entrectinib, an oral TKI, inhibits ROS1 & TRK. It has gone through several trials, including a phase 3 trial. Lorlatinib, a third-gen TKI, targets ALK & ROS1 positive NSCLC. Repotrectinib, a next-gen ROS1/TRK inhibitor, has a > 90-fold potency against ROS1 compared to crizotinib. Taletrectinib, a potent & selective ROS/NTRK inhibitor, has shown high effectiveness in phase I/II clinical trials.
NTRK gene fusion inhibitors
TRK gene fusion is a well-known oncogenic driver for solid tumors, like in the case of NSCLC. Both larotrectinib and entrectinib have been approved by the USFDA for NTRK gene fusions.
Another phase II study is also underway with repotrectinib.
KRAS inhibitors
KRAS is one of the earliest known oncogenic drivers in NSCLC. Despite that, effective targeting is still a therapeutic challenge. KRAS p.G12C mutation is seen in 13% of patients with NSCLC.
Sotorasib, a small molecule that inhibits KRAS G12C through P2 pocket interaction, has been tested on a phase II trial. Currently, a global phase III randomized study is underway.
Adagrasib, another small-molecule inhibitor of KRAS G12C, is being evaluated in a phase I/II study.
Drug antibody conjugates
Antibody-drug conjugates (ADCs) are now being studied for targeted therapy.
Patritumab deruxtecan has shown tolerable safety and antitumor activity in an ongoing study. Cofetuzumab pelidotin has shown great results in a phase I study, and a phase 1b study is underway. Carcinoembryonic antigen-related cell adhesion molecule 5 or CEACAM5 has gone through a first-in-human study, and a phase 3 trial is underway. TROP2 is going through an ongoing phase 1 study, and a phase 3 study is also underway.
PI3K/AKT/mTORC inhibitors
Lung cancer doctor in Delhi NCR, pan India, and abroad heavily implicate the PI3K/AKT/mTOR pathway in tumorigenesis & NSCLC disease progression.
Sapanisertib, an oral TORC1/2 inhibitor, has been evaluated in a phase II trial with stage IV squamous NSCLC patients recently. Sirolimus is another compound that is being studied in a phase I/II trial, and it binds to FKBP-12, an intracellular protein, forming an immunosuppressive complex that inhibits mTOR.
Gedatolisib, an intravenous ATP-competitive, pan-PI3K/mTORi, has demonstrated significant positive results in preclinical studies. A phase I clinical trial is currently recruiting.
RMC-5552, a bi-steric mTORC1-selective inhibitor, is currently being evaluated in a phase I/Ib, open-label, multicenter, dose-escalation trial as monotherapy in adults with certain types of NSCLC.
Nab-Rapamycin is being studied in a phase I/II trial combined with Nivolumab.
Epilogue
The future of targeted therapy for advanced non-small-cell lung cancer is bright. More and more studies are being conducted worldwide to make targeted therapy a mainstay treatment option for advanced NSCLC. We have mentioned some of the latest and future options in this blog. For more information, you can always consult an expert like Dr. Manish Singhal, the best cancer doctor in Noida specializing in lung cancer.



