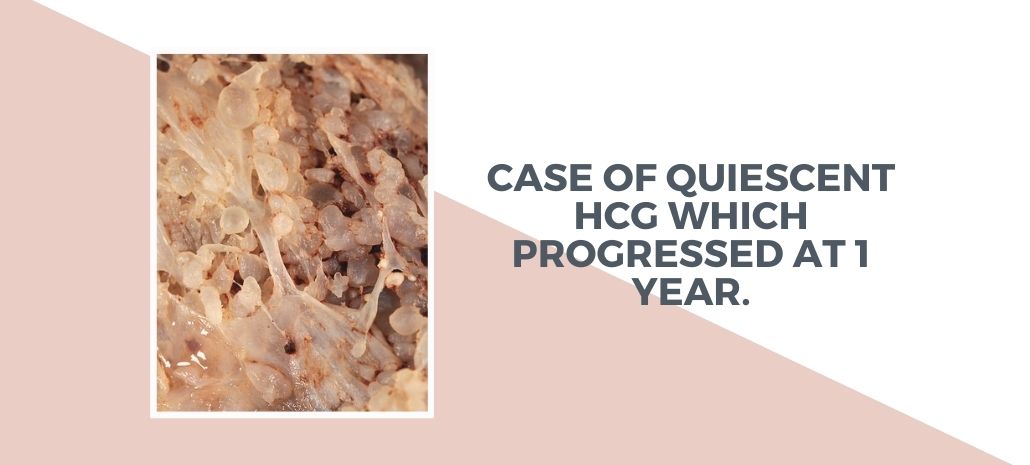
Mrs. AS was diagnosed as Complete Mole at age of 34. She had one living healthy child. She underwent suction and D&C with persistent elevation of bHCG warranting start of methotrexate the alternate day schedule with leucovorin rescue. Her bHCG normalized but elevated in 3 weeks and plateaued at 23.24 mIU/ml. She underwent a USG and Doppler pelvis and CT chest and abdomen which was reported unremarkable. There were 2 differentials – A False bHCG (Phantom or Pitutary) or a Quiescent bHCG.
Phantom bHCG –This false-positive test result occurs as a result of the presence of nonspecific heterophile antibodies in the patient’s serum, which cross-reacts in the HCG assay. False-positive hCG can be determined by
1) urine hCG assay , which will be negative because heterophile antibody is not excreted in the urine due to the large molecule size
2) serial dilution of the sample, as false hCG levels will remain largely unaffected by dilution
3) use of different commercial assays that will often result in significant fluctuation in the hCG level.
Pitutary bHCG – This false positive can be found in 1 % of perimenopausal and 7 % of postmenopausal women. This is due to raised levels of pituitary follicle-stimulating hormone and luteinizing hormone, as well as a benign low level of pituitary hCG secretion due to lack of feed back inhibition due to gonadal hormones. In the case of pituitary hCG, the production can be inhibited with oral contraceptive pills or using LHRH antagonist such as degarelix.
Quiescent bHCG– Usually the hCG level is in the range of 50–100 mIU/mL and remains static for at least 3 months. It is associated with a prior history of GTD or spontaneous abortion and does not respond to therapy. This condition is thought to occur when a small focus of dispersed, differentiated syncytiotrophoblast cells are present. These slow-growing syncytiotrophoblast cells produce small stable amounts of hCG and do not usually progress to invasive disease as long as the cytotrophoblast, or intermediate cells, are absent. These syncytiotrophoblast cells do not respond to chemotherapy as they are extremely slow-growing and does not result in normalization of hCG.
Hypergylcosylated hCG (hCG-H) measurement – glycoprotein produced by cytotrophoblast cells and is associated with trophoblast invasion, growth of cytotrophoblast cells, and is the main form of hCG produced in active choriocarcinoma and gestational trophoblastic neoplasm.The USA HCG Reference Service has demonstrated that the proportion of hCG-H (hCG-H / total hCG) is a 100 % sensitive marker for distinguishing active GTN/ choriocarcinoma from quiescent GTD.
Approximately 20 % of patients with quiescent GTD will start to produce increased hCG after a period of several weeks to years. During the quiescent period, the hCG-H is undetectable, but once the hCG rises, a significant proportion is hCG-H; this is often noted before the appearance of clinically detectable disease.
She was kept under follow up and remained well for almost a year when her bHCG shot up to 1,47,000mIU/ml. MRI Abdomen showed infiltrative lesion in uterus of 6 cm and NCCT chest was normal. Her risk score was 7 favoring a multiagent chemotherapy protocol with EMACO. Post 3 cycles her bHCG normalised. She received 2 more cycles post normalization. And preferred to get an hysterectomy done as she didn’t want to preserve fertility. Her case highlights a case of Quiescent HCG which progressed at 1 year.
Reference:
1. Siew-Fei Ngu & Karen K. L. Chan: Management of Chemoresistant and Quiescent Gestational
Trophoblastic Disease. Curr Obstet Gynecol Rep (2014) 3:84–90