Dr Manish Singhal - The best Cancer Specialist in Delhi
Brain Cancer Doctor In Noida
Brain Cancer (Tumor)
Cerebrum tumor is an ailment of the mind in which cancer cells emerge in the brain tissue. Cancer cells develop to frame a mass of cancer tissue (tumor) that meddles with brain capacities, for example, muscle control, sensation, memory, and other typical body capacities. Tumors made out of cancer cells are called threatening tumors, and those made out of primarily noncancerous cells are called favorable tumors. Cancer cells that create from brain tissue are called essential brain tumors while tumors that spread from other body destinations to the mind are named metastatic or secondary brain tumors.
Reports propose that brain tumor happens rarely (1.4% of all new disease patients every year), so it isn’t thought to be a typical ailment and is probably going to create in around 23,770 new individuals for each year with around 16,050 deaths as assessed by cancer reports. Just around 5% of brain tumors might be because of inherited hereditary conditions, for example, neurofibromatosis, tuberous sclerosis, and a couple of others.
The treatment options for brain cancer or brain tumor have come a long way, bringing the 5-year survival rate to almost 36%. The Covid-19 pandemic has instilled fear and confusion among cancer patients regarding how to keep the treatment going through the pandemic, but missing treatment might not be the best option for most people. So, the best Oncologist in Noida and renowned cancer treatment doctor in Delhi NCR and, Dr. Manish Singhal and his team have found a solution to the looming problem, chemotherapy at home, video consultations, patient check-ins through calls, and more.
Types of Brain Cancers
Brain cancer is basically divided into two groups: Primary & Secondary tumors:
Primary Brain Tumors
Tumors that start inside brain tissue are known as primary mind tumors. They are characterized by the kind of tissue in which they emerge. The most well-known brain tumors are gliomas, which start in the glial tissue. There are a few kinds of gliomas, including:
Astrocytomas
Emerge from little, star-formed cells called astrocytes. They may develop anyplace in the brain or spinal code. In grown-ups, astrocytomas regularly emerge in the brain. In youngsters, they happen in the brain stem, the cerebrum, and the cerebellum. A review III astrocytoma is some of the time called anaplastic astrocytoma. A review IV astrocytoma is normally called glioblastoma multiforme.
Oligodendrogliomas
Emerge in the cells that deliver myelin, the greasy covering that ensures nerves. These tumors as a rule emerge in the cerebrum. They develop gradually and ordinarily don’t spread into encompassing brain tissue.
Ependymomas
The most part develops in the coating of the ventricles. According to the best Oncologist in Noida, they may likewise happen in the spinal cord. In spite of the fact that these tumors can create at any age, they are most regular in childhood.
There are different sorts of brain tumors that don’t start in glial tissue. Probably the most widely recognized are:
- Meningiomas-Develop from the meninges. They are normally kind. Since these tumors become gradually, the brain might have the capacity to change in accordance with their presence. Meningiomas may become very extensive before they cause any kinds of symptoms. They happen frequently in ladies between 30 and 50 years old.
- Schwannomas-Benevolent tumors that emerge from Schwann cells, which create the myelin that ensures fringe nerves. Acoustic neuromas are a kind of schwannoma. They happen for the most part in grown-ups. These tumors influence ladies twice as frequently as men.
- Craniopharyngiomas-Create in the locale of the pituitary organ close to the hypothalamus. They are typically kind; however, they are some of the time considered harmful in light of the fact that they can press on or harm the hypothalamus and influence essential capacities. These tumors happen frequently in youngsters and youths.
- Germ cell tumors-Emerge from crude (creating) sex cells or germ cells. The most regular sort of germ cell tumor in the brain is a germinoma.
- Pineal district tumors-Happen in or around the pineal organ, a minor organ close to the focal point of the mind. The tumor can be moderate developing (pineocytoma) or quickly developing (pineoblastoma). The pineal area is extremely hard to reach, and these tumors regularly can’t be expelled
Secondary Brain Tumors
Secondary brain tumors are caused by cancer that starts in another piece of the body. These tumors are not the same as primary brain tumors. The spread of cancer inside the body is called metastasis. Cancer that spreads to the brain is a similar sickness and has an indistinguishable name from the first (primary) tumor. For instance, if lung cancer spreads to the brain, the infection is called metastatic lung disease on the grounds that the cells in the optional tumor look like unusual lung cells, not irregular brain cells.
Brain cancer doctor in Delhi says, treatment for secondary brain tumors relies upon where cancer started and to which extent it has spread and in addition different variables, including the patient’s age, general health, and reaction to past treatment.
Know the Risk Factors
Despite the fact that risk factors regularly impact the development of a brain tumor, most don’t straightforwardly cause a brain tumor. A few people with risk factors never build up a brain tumor, while others with no known risk factors do. Knowing your risk factors and discussing them with your specialist may enable you to settle on more educated choices. However, right now, there are no known approaches to prevent brain tumors through lifestyle changes.
The following factors may raise a person’s risk of building up a mind tumor:
Age
Brain tumors are more typical in kids and older adults, in spite of the fact that individuals of all ages can build up a mind tumor.
Gender
Men are more probable than ladies to build up a brain tumor. In any case, some particular sorts of brain tumors, for example, meningioma, are more typical in ladies.
Home and work exposures
Exposure to solvents, pesticides, oil items, elastic, or vinyl chloride may expand the danger of building up a brain tumor. Nonetheless, there isn’t yet logical confirmation that supports this conceivable connection.
Family history
Around 5% of brain tumors might be connected to innate hereditary factors or conditions, including Li-Fraumeni disorder, neurofibromatosis, nevoid basal cell carcinoma disorder, tuberous sclerosis, Turcot disorder, and von Hippel-Lindau malady.
Exposure to contaminations, infections, and allergens
Disease with the Epstein-Barr infection (EBV) builds the danger of CNS lymphoma. EBV is all the more generally known as the infection that causes mononucleosis or “mono”. In other research, abnormal amounts of a typical infection called cytomegalovirus (CMV) have been found in brain tumor tissue.
Electromagnetic fields
Considering the opinion of the best oncologist in India and studies assessing the role of electromagnetic fields, for example, vitality from electrical cables or from mobile phones, demonstrate no connection to an expanded danger of building up a brain tumor in grown-ups. Yet, The World Health Organization (WHO) suggests limiting cell phone use and promotes the utilization of a hands-free headset for both grown-ups and kids.
Symptoms of Brain Cancer
Individuals with a brain tumor may encounter the following symptoms, as stated by a brain cancer doctor in Noida. Once in a while, individuals with a brain tumor don’t have any of these changes. Or on the other hand, the reason for a side effect might be an alternate medicinal condition that isn’t a brain tumor. Symptoms of a brain tumor can be general or particular. A general side effect is caused by the weight of the tumor on the brain or spinal cord. Particular side effects are caused when a particular piece of the mind isn’t functioning admirably in light of the tumor. For some individuals with a brain tumor, they were analyzed when they went to the specialist in the wake of encountering an issue, for example, a migraine or different changes.
General symptoms include:
- Headaches, which might be serious and compound with movement or in the early morning
- Seizures- Motor seizures, are sudden automatic developments of a person’s muscles. Individuals may encounter distinctive kinds of seizures, including myclonic and tonic-clonic (great mal). Certain medications can encourage forestall or control them.
- Home and work exposures- Exposure to solvents, pesticides, oil items, elastic, or vinyl chloride may expand the danger of building up a brain tumor. Nonetheless, there isn’t yet logical confirmation that supports this conceivable connection.
- Memory changes
- Vomiting
- Weakness
- Sleep issues
- Memory issues
- Changes in capacity to walk or perform day by day exercise
Symptoms that might be particular to the area of the tumor include:
- Weight or a migraine close to the tumor
- Changes in judgment, including loss of activity, laziness, and muscle shortcoming or loss of motion are related to a tumor in the frontal flap of the brain.
- Fractional or finish loss of vision is caused by a tumor in the occipital projection or transient flap of the brain.
- Changes in speech, hearing, memory, or passionate state, for example, forcefulness and issues understanding or recovering words can create from a tumor in the frontal and worldly flap of the brain.
- A modified impression of touch or weight, arm or leg shortcoming on 1 side of the body, or disarray with left and right sides of the body are connected to a tumor in the frontal or parietal projection of the brain.
- Powerlessness to look upward can be caused by a pineal organ tumor.
- Vision changes, including loss of part of the vision or twofold vision, can be from a tumor in the fleeting flap, occipital projection, or mind stem.
Brain Cancer Grading
The staging procedure surveys the spread of disease beyond the source site. A brain tumor doesn’t behave in the same way as other cancers. Tumors may relocate inside the brain, yet it is exceptionally uncommon for essential mind tumors to spread outside of the mind, or far from the central nervous system (CNS).
Therefore, a brain tumor is normally graded rather than staged. The brain tumor evaluating systems highlights four particular evaluations and furnishes your care group with a comprehension of how the tumor develops. This procedure enables our specialists to coordinate brain cancer to singular needs.
Evaluating brain tumors
To decide the development and improvement of tumors in the brain, the best oncologist in india center around the qualities of the tumor and its impact on usefulness. The fundamental elements used to survey brain tumors include:
- Size and location
- Kind of tissue or cells affected
- Resectability
- The spread of the tumor inside the brain or spinal code
- The possibility tumor has spread beyond the brain or CNS
An entire appraisal will likewise factor in age and any brain cancer side effects that are restricting essential capacities, for example, discourse, hearing or development. Brain cancer grading is entirely different from staging other tumors in the body. Cancers in the lung, colon and bosom are organized in view of their area in the body, estimate, lymph node involvement, and conceivable spread. Tumors in the brain are evaluated in view of how forceful the tumor cells show up under a microscope.
The grade and respectability of the tumor will help control treatment choices. The medical procedure relies upon the tumor’s openness (area), estimate, degree (spread inside the brain) and the patient’s general health.
Diagnosis
The best oncologist in India, use numerous tests to discover, or analyze a brain tumor and learn the type of brain tumor. They likewise do tests to learn if it has spread to another piece of the body from where it began. This is called metastasis and is uncommon for a brain tumor. Specialists may likewise do tests to realize which medicines could work best.
For most sorts of tumors, taking an example of the possible tumor is the main beyond any doubt route for the specialist to know whether an area of the body has a tumor. This might be done in a methodology called a biopsy or by evacuating part or the greater part of the tumor with medical procedure. In a biopsy, the specialist takes a little example of tissue for testing in a research facility. If that isn't conceivable, the specialist may recommend different tests that will help make a conclusion.
Imaging tests can enable specialists to see whether the tumor is a primary brain tumor or if it is growth that has spread to the brain from somewhere else in the body. Imaging tests indicate photos within the body. Your specialist may consider these variables while picking a diagnotic test.
Most brain tumors are not analyzed until after symptoms show up. Frequently a brain tumor is at first analyzed by an internist or a neurologist. An internist is a specialist who spends significant time in treating grown-ups. A neurologist is a specialist who spends significant time in issues with the mind and central nervous system.
With a detailed medical history, the specialist may suggest the following tests:
A MRI utilizes attractive fields, not x-rays, to deliver detailed pictures of the body. MRI can be utilized to measure the tumor’s size. An uncommon dye called a complexity medium is given before the sweep to make a clearer picture. This dye can be infused into a patient’s vein or given as a pill to swallow. MRI make more point by point pictures than CT scans and are the favored method to analyze a brain tumor. The MRI might be of the mind, spinal code, or both, depending upon the kind of tumor suspected and the probability that it will spread in the CNS.
A CT scan makes a 3-dimensional photo of within the body utilizing x-rays taken from various points. A PC joins these pictures into a point by point, cross-sectional view that demonstrates any anomalies or tumors. A CT output can help discover draining and development of the liquid filled spaces in the brain, called ventricles. Changes to the bone in the skull can likewise be seen on a CT output, and it can be utilized to gauge a tumor’s size. A CT scan may likewise be utilized if the patient can’t have an MRI, for example, if the individual has a pacemaker for his or her heart. Once in a while, a complexity medium is given before the scan to give better detail on the picture. This dye can be infused into a patient’s vein or given as a pill to swallow.
A PET scan is utilized at first to discover more about a tumor while a patient is accepting treatment. It might likewise be utilized if the tumor returns after treatment. A PET scan is normally joined with a CT scan, called a PET-CT check. However, you may hear your specialist allude to this methodology similarly as a PET scan. A PET scan is an approach to make pictures of organs and tissues inside the body utilizing different substances, for example, sugars or proteins. A little measure of a radioactive substance is infused into the patient’s body. This substance is taken up by cells that are currently isolating. Since tumor cells will probably be currently separating, they ingest a greater amount of the radioactive substance. A scanner at that point distinguishes this substance to create pictures of within the body.
A biopsy can be executed as a major aspect of a task to evacuate the brain tumor, or a biopsy can be performed utilizing a needle.
A stereotactic needle biopsy might be done for brain tumors in difficult to achieve territories or extremely touchy regions inside your mind that may be harmed by a more broad activity. Your neurosurgeon penetrates a little gap into your skull. A thin needle is then embedded through the gap. The tissue is evacuated utilizing the needle, which is as often as possible guided by CT or MRI checking. The biopsy test is then seen under a magnifying instrument to decide whether it is carcinogenic or benevolent. Advanced research center tests can give your specialist signs about your prognosis and your treatment choices.
Treatment
Treatment for a brain tumor relies upon the type, size and area of the tumor, and in addition your general health and your inclinations.
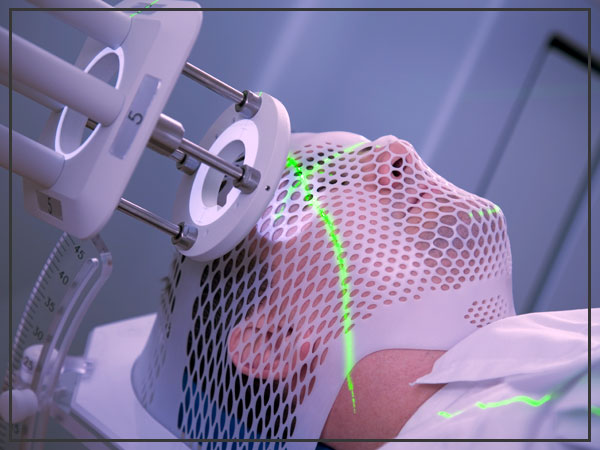
Radiation therapy
Radiation therapy utilizes high-vitality beams, for example, X-rays or protons, to murder tumor cells. Radiation treatment can originate from a machine outside your body (outer pillar radiation), or, in extremely uncommon cases, radiation can be put inside your body near your brain tumor (brachytherapy).
External beam radiation can concentrate just on the territory of your mind where the tumor is found, or it can be connected to your whole brain. Entire brain radiation is regularly used to treat a disease that spreads to the brain from some other piece of the body and structures numerous tumors in the cerebrum.
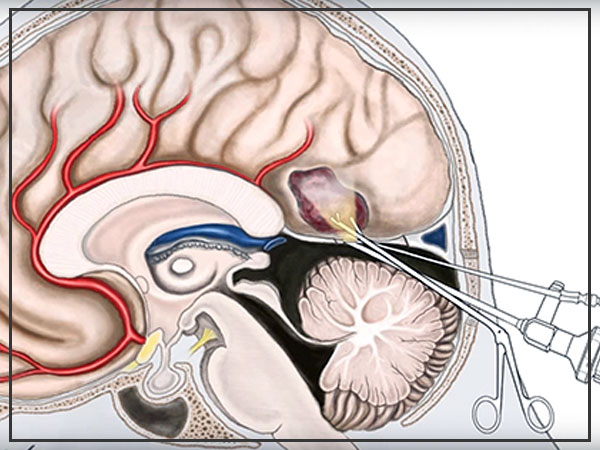
Surgery
If a brain tumor is situated in a place that makes it open for an operation, your specialist will work to expel however much of the brain tumor as could reasonably be expected. Sometimes, tumors are little and simple to isolate from encompassing brain tissue, which makes finish careful expulsion conceivable. In different cases, tumors can’t be isolated from encompassing tissue or they’re situated close to touchy regions in your brain, making medical procedure dangerous. In these circumstances, your specialist expels as a significant part of the tumor as is protected. Even evacuating a bit of the cerebrum tumor may help decrease your signs and manifestations.
Surgery to expel a brain tumor conveys dangers, for example, contamination and dying. Different dangers may rely upon the piece of your mind where your tumor is found. For example, surgery on a tumor close to nerves that associate with your eyes may convey a danger of vision loss.
Radiosurgery
Stereotactic radiosurgery isn’t a type of medical procedure in the customary sense. Rather, radiosurgery utilizes various light emissions to give an exceedingly engaged type of radiation treatment to execute the tumor cells in a little territory. Each light emission isn’t especially intense, yet the point where every one of the shafts meets at the brain tumor gets a substantial dosage of radiation to kill the tumor cells.

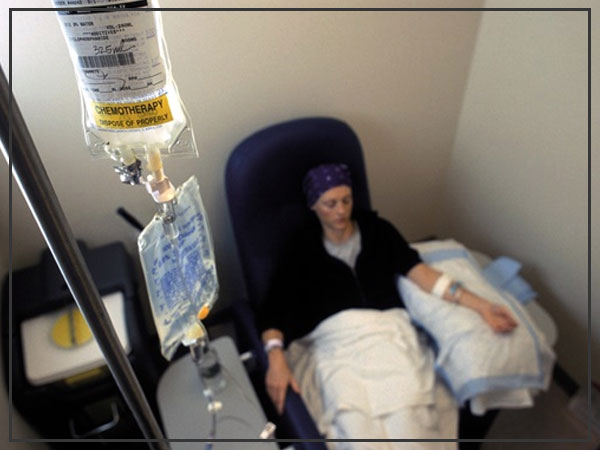
Chemotherapy
Chemotherapy utilizes medications to execute tumor cells. Chemotherapy medications can be taken orally in pill frames or infused into a vein (intravenously). The chemotherapy drug utilized frequently to treat mind tumors is temozolomide (Temodar), which is taken as a pill. Numerous other chemotherapy drugs are accessible and might be utilized relying upon the kind of cancer.
Recovery after treatment
Speech instruction session
Since brain tumors can create parts of the mind that control engine abilities, discourse, vision and consideration, restoration might be a fundamental piece of recovery. Depending upon your necessities, your specialist may allude you to:
Non-intrusive treatment to enable you to recapture lost motor abilities or muscle quality
Word related treatment to enable you to return to your ordinary day by day exercises, including work, after a cerebrum tumor or different ailment
Language instruction with experts in discourse troubles (discourse pathologists) to help in the event that you experience issues talking
Coaching for school-age kids to enable children to adapt to changes in their memory and thinking after a brain tumor.
Prevention
The danger of many tumors in grown-ups can be lessened with certain way of life changes, (for example, maintaining a healthy weight or quitting smoking). However, other than radiation exposure, there is no known way of life related or ecological risk factors for brain and spinal cord tumors, so as of now there is no known method to secure against the majority of these tumors.



