Dr Manish Singhal - The best Cancer Specialist in Delhi
Pancreatic Cancer in Noida, Delhi NCR
Pancreatic Cancer
Pancreatic cancer accounts for 7% of all cancer deaths. Developed countries around the world account for most of those deaths. Before diving deeper into the why and what of pancreatic cancer, we must consider the effect of the Covid-19 pandemic on pancreatic cancer treatment and management plans. All oncologists are doing something or the other to adapt, but only some ways are proving to be successful. Dr. Manish Singhal, the best cancer treatment doctor in Delhi NCR, is offering chemotherapy at home and other telemedicine services successfully while taking all the preventive measures necessary at the moment.
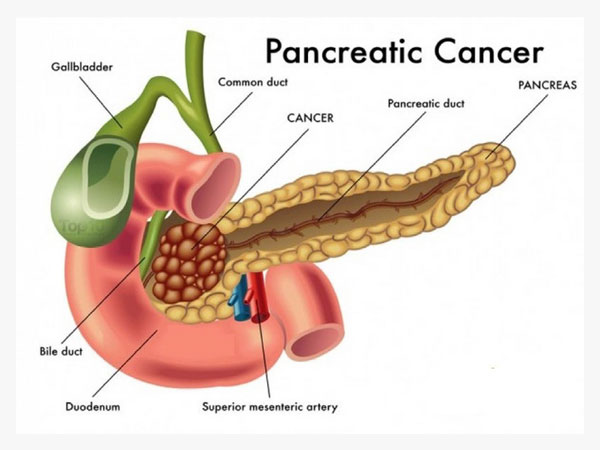
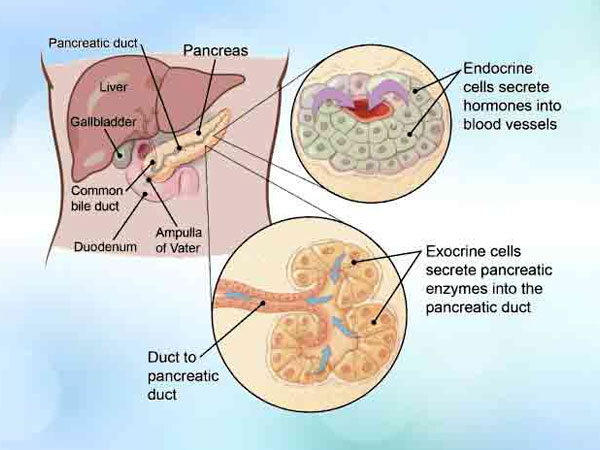
The pancreatic disease begins when cells in the pancreas begin to become out of control. The pancreas is an organ that sits behind the stomach. It’s molded somewhat like a fish with a wide head, a decreasing body, and a tight, pointed tail. In grown-ups, it’s around 6 inches in length however under 2 inches wide. The leader of the pancreas is on the correct side of the midriff (tummy), behind where the stomach meets the duodenum (the initial segment of the small digestive system). The body of the pancreas is behind the stomach, and the tail of the pancreas is on the left half of the belly alongside the spleen. The pancreas has 2 primary types of cells:
Exocrine cells
Most of the cells in the pancreas frame the exocrine organs and pipes. The exocrine organs make pancreatic compounds that are discharged into the digestive tracts to enable you to process nourishments (particularly fats). The chemicals are first discharged into modest tubes called conduits. These converge to shape larger ducts, which void into the pancreatic pipe. The pancreatic duct converges with the normal bile pipe (the pipe that conveys bile from the liver) and purges into the duodenum (the initial segment of the small digestive tract) at the ampulla of Vater.
Endocrine cells
Endocrine cells make up a substantially little level of the cells in the pancreas. These cells are in little bunches called islets (or islets of Langerhans). These islets make vital hormones like insulin and glucagon (which enable control to glucose levels) and discharge them directly into the blood.
Types of Pancreatic Cancer
The exocrine cells and endocrine cells of the pancreas make diverse kinds of tumors. It’s imperative to know whether the tumor in the pancreas is an exocrine or endocrine cancer. They have different risk factors and causes, have distinctive signs and side effects, are determined to have diverse tests, are dealt with in various ways, and have distinctive standpoints.
Exocrine pancreatic cancers
Exocrine cancers are by a wide margin the most well-known kind of pancreas cancer. If you are told that you have pancreatic cancer it’s most likely an exocrine pancreatic cancer.
Pancreatic adenocarcinoma: About 95% of tumors of the exocrine pancreas are adenocarcinomas. These diseases, as a rule, begin in the pipes of the pancreas. Less often, they create from the glands that produce the pancreatic proteins, in which to case they are called acinar cell carcinomas.
Less basic kinds of exocrine cancer: Other, less normal exocrine cancer include adenosquamous carcinomas, squamous cell carcinomas, seal ring cell carcinomas, undifferentiated carcinomas, and undifferentiated carcinomas with monster cells.
Ampullary tumor (carcinoma of the ampulla of Vater): This one begins in the ampulla of Vater, which is the place the bile pipe and pancreatic pipe meet up and void into the small digestive tract. Ampullary growths aren’t actually pancreatic malignancies, however, they are incorporated here in light of the fact that they are dealt with much the same.
Ampullary tumors frequently obstruct the bile pipe while they’re still little and have not spread far. This blockage makes bile develop in the body, which prompts yellowing of the skin and eyes (jaundice). Also, these growths are normally discovered sooner than most pancreatic diseases, and they, for the most part, have a superior outcome (viewpoint).
Pancreatic endocrine tumors (Neuroendocrine Tumors)
Tumors of the endocrine pancreas are extraordinary, making up under 5% of every single pancreatic malignancy. As a group, they are regularly called pancreatic neuroendocrine tumors (NETs) or islet cell tumors.
Pancreatic NETs can be low grade or high grade tumors. High grade tumors are generally detected when it spreads outside the pancreas which is usually liver.
Risk Factors
A risk factor can affect your chance of having a disease such as cancer. Different cancers have different risk factors. Some of them like smoking can be changed. Others, like a person’s age or family history, can’t be.
But having a risk factor or even many does not imply that you will definitely get the disease. And many individuals who get it may have few or no known risk factors. Several factors can affect a person’s chance of getting cancer of the pancreas. Many of these are risk factors for exocrine pancreatic cancer.
Age
The danger of creating a pancreatic disease goes up as individuals age. All patients are more established than 45. Around 66% are no less than 65 years of age
Stomach issues
Infection of the stomach with the ulcer-causing microscopic organisms Helicobacter pylori (H. pylori) may build the danger of getting a pancreatic tumor. Best Oncologist in Delhi has recommended that overabundance stomach corrosive may likewise expand the risk.
Family history
Pancreatic cancer seems to run in some families. In some of these families, the high risk is due to an inherited syndrome. In other families, the gene causing the increased risk is not known. Although family history is a risk factor, most people who get pancreatic cancer do not have a family history of it.
Gender
Men are somewhat more inclined to create pancreatic cancers than ladies. This might be expected looking at the higher tobacco use in men, which raises pancreatic disease chance.
Chronic pancreatitis
Chronic pancreatitis, a long haul irritation of the pancreas, is connected with an expanded danger of pancreatic growth (particularly in smokers), however, many people with pancreatitis never create pancreatic disease.
Diabetes
The pancreatic disease is more typical in individuals with diabetes. The purpose behind this isn’t known. The greater part of the risk is found in individuals with type 2 diabetes. This sort of diabetes frequently begins in adulthood and is regularly identified as being overweight or fat. It’s not clear if individuals with type 1 (adolescent) diabetes have a higher risk.
The symptoms of exocrine pancreatic cancers and pancreatic neuroendocrine tumors (NETs) are regularly extraordinary, so they are depicted independently. Having at least one of the indications underneath does not mean you have a pancreatic tumor. Truth be told, a considerable lot of these symptoms will probably be caused by different conditions. Still, if you have any of these side effects, it’s critical to have them checked by a specialist so that the reason can be found and treated if necessary.
Symptoms
Jaundice
Jaundice is caused by the development of bilirubin, a dull yellow-darker substance made in the liver. Typically, the liver discharges bilirubin as a major aspect of a fluid called bile. Bile experiences the basic bile conduit into the digestive tracts, where it helps separate fats. It, in the long run, leaves the body in the stool. At the point when the normal bile conduit winds up blocked, bile can’t achieve the digestive tracts, and the level of bilirubin in the body develops.
Back pain
Pain in the stomach area or back is normal in pancreatic disease. Cancers that begin in the body or tail of the pancreas can become genuinely substantial and begin to push on other close-by organs, causing pain. A tumor may likewise spread to the nerves encompassing the pancreas, which frequently causes back pain. Obviously, pain in the belly or back is genuinely normal and is regularly caused by an option that is other than pancreatic cancer.
Nausea
If cancer presses on the far end of the stomach it can partly block it, making it hard for food to get through. This can cause nausea, vomiting, and pain that tend to be worse after eating.
Weight loss and poor appetite
Unexpected weight loss is very common in people with pancreatic cancer. These people often have little or no appetite.
Stages
Staging is a method for portraying where the cancer is found, if or where it has spread, and whether it is influencing different parts of the body. Specialists use symptomatic tests to discover the cancer stage, so staging may not be finished until the point when every one of the tests is done. Knowing the stage helps the specialist to choose what sort of treatment is ideal and can help foresee a patient’s survivability which is the possibility of recuperation. There are distinctive stage portrayals for various sorts of the tumor. It is vital for the organizing to be from a medicinal focus with involvement in arranging pancreatic growth.
This kind of pancreatic cancer can be precisely evacuated. Surgery is frequently done directly after the diagnosis. Some of the time, extra treatment might be prescribed before medical procedure. The tumor might be found just in the pancreas or reach out past it, however it has not developed into imperative conduits or veins in the territory. There is no confirmation that the tumor has spread to zones outside of the pancreas. Around 10% to 15% of patients are determined to have this stage.
This portrays a tumor that might be troublesome or unrealistic to evacuate precisely when it is first analyzed, however, if chemotherapy or potentially radiation treatment can contract the tumor to start with, it might have the capacity to be expelled later with negative edges. A negative edge implies that no unmistakable malignancy cells are abandoned.
The tumor has spread past the region of the pancreas and to different organs, for example, the liver, lungs, or inaccessible parts of the mid-region. Around 45% to 55% of patients are diagnosed to have this stage.
Specialists use a few systems to arrange pancreatic disease. The technique used to arrange different cancers, called the TNM system. However, it isn’t frequently used for pancreatic tumor; but for the other cancers.
Treatment
Surgery
Two general kinds of surgery can be utilized for pancreatic cancer.
Potentially curative surgery is utilized when the aftereffects of exams and tests propose that it’s conceivable to remove all cancer.
Palliative surgery may be done if imaging tests demonstrate that the cancer is too across the board to ever be removed totally. This medical procedure is done to mitigate symptoms or to keep certain complexities like a blocked bile conduit or digestive tract, yet the objective isn’t to attempt to fix cancer.

Ablation or Embolization Treatments for Pancreatic Cancer
Ablation or Embolization Treatments can some of the time be used to help treat the pancreatic disease that has spread to different organs, particularly the liver. However, these medications are probably not going to fix diseases all alone. They will probably be utilized to help counteract or diminish side effects, and are frequently used alongside different kinds of treatment.
Radiation Therapy
Radiation therapy can be useful in treating some exocrine pancreatic tumors (the most well-known sort of pancreatic cancer). Radiation may be given after surgery to attempt to bring down the chance of cancer returning. The radiation is normally given alongside chemotherapy, which is as one known as chemoradiation or chemoradiotherapy.
Chemotherapy
Chemotherapy (chemo) uses hostile to disease drugs infused into a vein or taken by mouth. These medications enter the circulatory system and reach all zones of the body, making this treatment possibly valuable for diseases that have spread past the organ they began in.
According to the Cancer Specialist in Delhi, Pancreatic neuroendocrine tumors (NETs) don’t react well to radiation, so rarely do use to treat these tumors. Radiation is in some cases used to treat pancreatic NETs that have spread deep down and are causing pain It might likewise be used as a part of the type of radioembolization to treat NETs that have spread to the liver, which was talked about in Ablation or Embolization Treatments for Pancreatic Cancer.

Prevention
There is no certain method to prevent pancreatic tumor. Some risk factors, for example, age, sex, race, and family history can’t be controlled. However, there are things you can do that may bring down your danger such as:
- Quit smoking
- Eat Well
- Exercise regularly
- Limit alcohol use
Contact the Best Oncologist in Delhi to get to know more about pancreatic cancer and it’s treatments.



